Most modern healthcare systems face overwhelming odds to serve their communities. Reduced or quality-driven reimbursements from payers, historic inflation levels, increasing demand from an aging population and public scrutiny create immense pressure to control costs, streamline operations and improve patient outcomes. This cultivates an environment where workforce optimization strategies often become polarizing and contentious, leading to decisions that prioritize immediate cost savings as a matter of survival.
One such approach is the complete elimination of contingent workforce usage, pursued in the belief that it will reduce overall labor expenses. However, as healthcare’s largest workforce (nursing) evolves, this strategy often backfires, triggering unintended consequences such as inadequate or unsafe staffing perceptions, core staff burnout, increased turnover and refractory overreliance on contract labor to avoid bed closures and lost revenue. This vicious cycle not only proves financially unsustainable but also undermines workforce agility and fails to meet the flexibility demands of today’s healthcare professionals.
Moreover, zero contingent workforce budgeting diverges sharply from best practices in workforce management science, which emphasizes balancing core and contingent staff to optimize flexibility, efficiency and outcomes. In this article, we will explore the implications, consequences and alternative best practice suggestions to consider instead.
Why “total elimination of contract labor use” isn’t a sustainable cost savings strategy
1. Reduced workforce agility
Healthcare is inherently unpredictable. From seasonal surges like flu season, to unexpected crises such as pandemics or natural disasters, healthcare systems require staffing models that can respond quickly and efficiently. Contract labor is a critical lever to address these unplanned needs, especially for healthcare organizations whose full-time equivalent (FTE) budget and staffing plans are predicated on historical average daily census at less than the 75th peer benchmark percentiles. Eliminating contract labor without alternative contingencies in place leaves organizations with unpredictable and rigid staffing response models that struggle to adapt to variability. This lack of agility can result in operational bottlenecks, increased patient wait times and diminished quality of care.
2. Diminished talent flexibility
Today’s workforce increasingly values flexibility. Healthcare professionals, especially millennials and Gen Z workers, are drawn to roles that align with their personal and professional goals, such as per diem, seasonal or travel arrangements. By removing these options, healthcare systems risk alienating a significant segment of the existing talent pool and missing out on untapped staffing resources that are interested in working within more nimble programs, driving up voluntary turnover among permanent staff.
3. Financial implications
While the intention of eliminating contract labor is to cut costs and may be successful in the short term, it often results in the opposite in the long term. Overworked permanent staff face burnout, which leads to increased absenteeism, higher turnover and the need for costly overtime, expedited hiring processes and rapid response travel nurses at a premium rate. Additionally, lower staff morale often correlates with decreased patient satisfaction and outcomes, potentially impacting reimbursement rates and organizational reputation.
Unintended and refractory consequences
When healthcare organizations attempt to eliminate contract labor in totality, they often face a series of unintended and self-perpetuating challenges:
1. Increased burnout and turnover among core staff
Without contingent workers to alleviate the burden during high-demand periods, permanent staff are forced to work longer shifts, take on additional responsibilities and cope with heightened stress. Over time, this leads to higher rates of burnout, absenteeism and turnover—creating a vicious cycle where remaining staff are further burdened and begin to seek alternative, more flexible work options, leading them to exit organizations that do not offer these options. Recent findings show that over the past five years, cumulative average turnover among medical surgical, stepdown, telemetry and emergency nurses to be estimated at 115%, according to a 2024 NSI analysis.
2. Erosion of patient care quality
Staff burnout and understaffing directly impact patient care. Exhausted staff are more prone to errors, delays in treatment, and lapses in communication. Patient satisfaction scores decline, and nursing driven quality metrics decrease, and hospital acquired injury increases; potentially affecting CMS reimbursement and the hospital's overall reputation, according to Press Ganey.
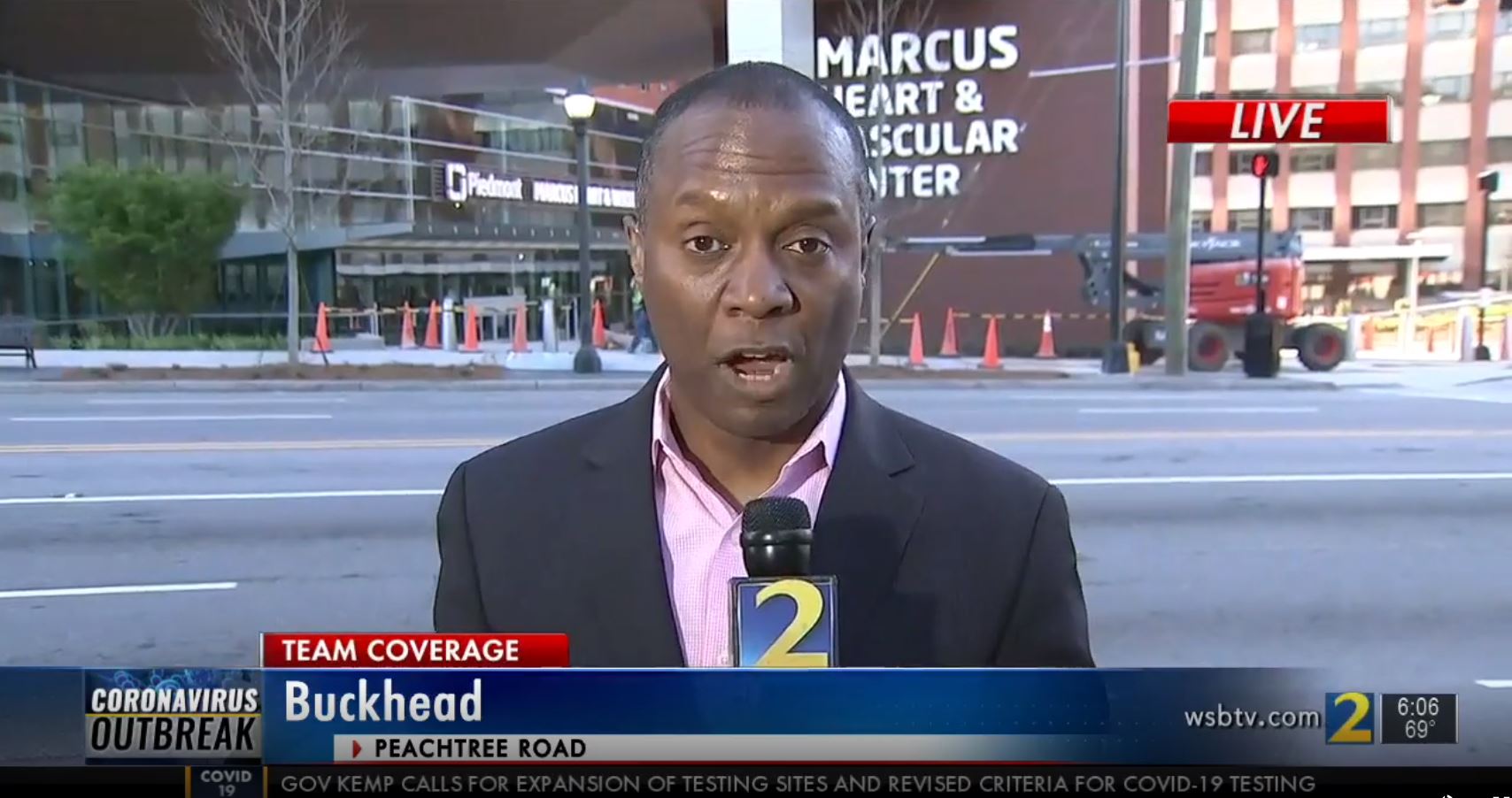
3. Inability to respond to crises
Healthcare crises—such as pandemics or mass casualty events—often require a surge workforce. Without access to a robust contingent workforce, healthcare systems are left scrambling to fill gaps, frequently resorting to costly and inefficient last-minute solutions. This not only strains finances but can also compromise the system’s ability to deliver timely, high-quality care. Prevalence of this phenomenon initiated the dramatic demand for travel nurses during the COVID-19 pandemic, leading to unprecedented increases in traveler bill and pay rates on a national scale.
4. Higher long-term costs and lost revenue
Eliminating contract labor doesn’t eliminate the need for flexible staffing—it merely shifts the cost burden and creates missed revenue opportunities in the short term. Organizations often find themselves paying more in overtime wages, expedited hiring costs, and/or closing licensed beds, suspending service offerings, or shuttering service lines altogether as a result on inability to fill staffing gaps. Studies have shown that reactive hiring practices can be 1.5–2 times more expensive than maintaining a well-managed contingent workforce, Modern Healthcare reported in 2022. According to the American Nurses Association, turnover can cost healthcare systems up to $88,000 per nurse annually in replacement and onboarding costs in addition to the contract labor expenses for covering staffing absence.
5. Deterioration of employer brand
Lack of nimble staffing model offerings that overworks permanent staff and provides no alternative options for flexibility can harm an organization's reputation as an employer. Recruitment conundrums such as the need to add non-budgeted human capital to talent acquisition teams to manage higher open requisition load, prolonged post-to-fill times and increased negotiations for higher compensation to offset lack of flexibility can make it increasingly difficult to attract top talent in a competitive labor market, further exacerbating staffing shortages, according to KPMG.
Best practices for healthy contingent workforce utilization
A more sustainable and effective strategy is to diversify the contingent workforce pipeline and harness its potential thoughtfully. Here are key suggestions for optimizing fiscally sustainable contingent workforce usage:
1. Develop an internal contingent workforce
Cultivating internal or “insourced” contingent resource pool options allows organizations to achieve maximum flexibility while reducing reliance on external staffing agencies. This can include creating or accessing existing per diem pools, float teams at the facility and enterprise level, or seasonal staffing programs. Internal contingent staff are often more cost-effective than external agency workers and can align closely with the organization’s culture and care standards.